The cure to celiac disease could be found in RNA sequencing, a technique where biologists analyze RNA to determine the level of gene expression, which has proven to be a valuable tool in determining which genes are important in finding treatment for celiac disease.
There is currently no cure, and the only existing treatment is a gluten-free diet. However, the emergence of new techniques to analyze the molecular impact of this disease has opened the door to effective drug development, giving people like me hope that we may one day feast on a banquet of all things gluten and delicious.
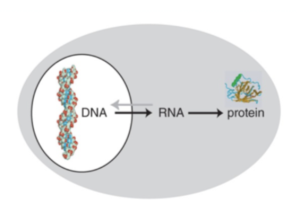
As you may have guessed, me having celiac disease has to do with my genetics. Our genes are extremely influential in dictating how our bodies function. You may recall from freshman biology class that our DNA is transcribed into RNA, which is translated to a protein. These proteins then do pretty much everything our body needs, from digesting food to communicating with other cells.
But when the DNA mutates, the resulting protein also changes. In the case of celiac disease, the mutated genes are called HLA-DQ2 and HLA-DQ8; both produce a protein that is extremely sensitive to gluten, binding to it more tightly and making it more likely to activate the immune system and cause irreparable damage to the body.
This is why many people with celiac experience stomach pain after ingesting gluten; their small intestine has become inflamed. Basically, celiac disease is caused by a genetic mutation that results in an oversensitivity to gluten.
So, the mystery of celiac disease is solved! Not really. Among people who have the mutated genes (HLA-DQ2 or HLA-DQ8), only about 3% actually have celiac disease. Something else has to be in play. A good way to understand the genetic differences between people who are affected by the disease and people who are unaffected is to analyze both of their DNA sequences and compare them. However, the human genome is enormous, and this would be a very lengthy and expensive process.
Instead, biologists take a single cell and study the all RNA sequences produced, called the transcriptome. This is important because some genes are never transcribed into RNA, meaning they are never expressed, while some genes are continually being transcribed into RNA, meaning they are constantly being expressed.

To determine which genes these are, each RNA sequence is matched to the corresponding DNA sequence in the human genome, a process called RNA sequencing. A gene that is expressed frequently will have lots of RNA sequences matched to it, while a gene that is never expressed won’t have any matches.
When RNA sequencing is applied to an affected individual and an unaffected individual, we can clearly see the differences in the levels of gene expression. For example, if the unaffected person has low levels of expression of gene X while the affected person has high levels of expression of gene X, then gene X may be important to the development of that disease.
These genes can become effective targets of drugs aiming to cure celiac disease. For example, by sequencing the RNA of HIV-infected T-cells, researchers were able to discern markers of that infection. This allowed them to better understand what HIV infection looks like at the molecular level, enabling them to identify all affected cells in a region and eliminate them, preventing further spread.
As more and more people are diagnosed with celiac every year, the impact of an effective cure grows. Currently, I’m using this exact process to better understand the genetic background of celiac disease. Food is a huge part of how we connect with each other, and developing a drug to cure celiac could help people like me gain access to more foods and live a more vibrant life.

